
In about 5-10% of cases, lateral lymph node metastases may skip the central neck, usually in patients where the tumor is located in the upper poles of the thyroid. more than half of the microscopic lymph node metastases were found in the lateral compartment.
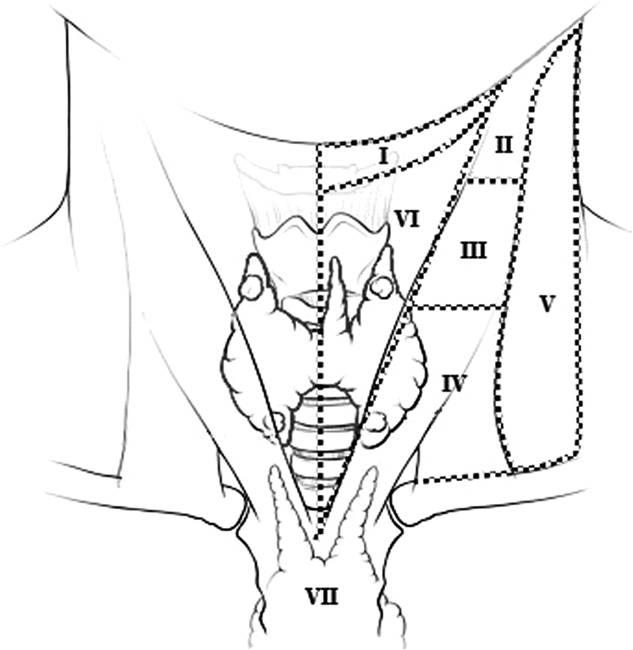
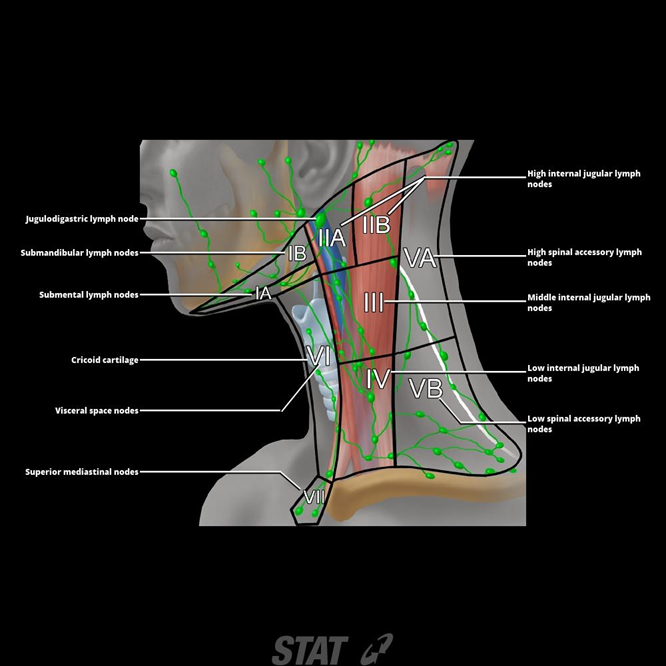
Lymphatic metastases are also commonly observed in the lateral compartment (most commonly to levels III and IV). About two-thirds of patients with PTC > 1 cm will have lymph node metastases in compartment VI, although in only half of these will the metastases be obvious to the naked eye. Lymph node metastases are commonly observed in the central compartment (level VI). Current evidence suggests specific patterns of lymphatic metastasis in PTC. Papillary thyroid carcinoma (PTC) frequently metastasizes to cervical lymph nodes, and a significant percentage of patients (up to 50-60% or even 90% for occult metastases) already have lymphatic spread at the time of diagnosis. Patterns of Lymph Node Metastasis in DTC and Clinical Implications CCA = Common carotid artery IJV = internal jugular vein. We routinely use this schematic lymphatic mapping in patients with thyroid cancer in the operating room (in close collaboration with our experienced radiologist, coauthor no. This graphic is based on ultrasonographic findings. Schematic representation of lymphatic mapping of the neck in a patient with thyroid cancer. The classification of cervical lymph nodes is schematically described in figure 1. Sublevel classification is also used when certain zones within the larger levels have independent biologic significance. This classification system is composed of 7 major nodal regions (levels or compartments I-VII) and defines a compartment-oriented neck dissection. This schema was later modified (in 20) and has become universally accepted (table 1). The first classification system for neck dissections was published in 1991 by the American Academy of Otolaryngology-Head and Neck Surgery. Modern classification of neck lymph nodes, based on findings and landmarks from cross-sectional anatomic imaging, is very useful in mapping nodal surgical intervention. The neck contains a very rich lymphatic network.

The aim of this brief report is to summarize currently available data regarding the patterns of cervical lymph node metastasis in patients with DTC clinical implications for the practicing surgeon will be briefly discussed, with a particular emphasis on the emerging role of compartment-oriented (so-called ‘selective') CLND, based on the findings of preoperative ultrasonographic lymphatic mapping. Accurate knowledge of these metastatic patterns, in addition to a detailed and reliable preoperative ultrasonographic lymphatic mapping of the neck, will allow a more selective and rational therapeutic approach in patients with DTC and lymph node metastases, thereby avoiding routine extensive dissections and their associated increased morbidity. Occasionally, skip metastases can occur, but in general lymphatic dissemination occurs in a stepwise fashion. Despite the continuing controversy regarding the role of prophylactic cervical lymph node dissection (CLND) in patients with DTC, it is widely accepted that in the presence of cervical lymphadenopathy CLND is indicated at the time of initial thyroidectomy. Lymphatic metastases at the time of diagnosis are common in differentiated thyroid cancer (DTC).


 0 kommentar(er)
0 kommentar(er)
